Data Sheet

Accountable Care Organization (ACO)
Acclivity provides the analytics, reporting, and dashboards to help ACOs succeed under MSSP and ACO REACH payment models.
ACO Reach
-
Risk Adjustment, Leakage, and Network Management Tools
Gain insights and take action on reporting and dashboards specific to uncovering, predicting and managing existing and future risk.
Easily uncover patients in real-time using out of network providers and deploy resources to prevent further leakage.
Uncover more insights into your current network to make the best decisions regarding providers and care.
-
Advanced Data Aggregation
With no IT lift on your end, we expediently unify all existing data including clinical, social determinants of health, claims, payment, other technologies and more into your EMR. All future data is automatically ingested to drive efficiency and reduce administrative burden. Everything is merged in single data visualization layer for seamless view into ACO REACH insights.
-
Predictive Analytics and Care Management Automation
Easily predict and manage current and future costs, risk, leakage, transitional care opportunities, chronic care cases, hospice and palliative eligibility, utilization, SDOH, mortality scores, health equity, and more.
-
Social Determinants of Health, Health Equity, and Post Acute Networks
Leverage our nationally recognized SDOH analysis tool that leverages census block analytics to identify social factors within a very specific census tract for that address. Plus, gain various health equity and behavioral health insights and predictive models to help ensure equal outcomes for all.
Access Acclivity’s hospice & palliative partners to reduce risk by enabling providers in your network to seamlessly transition end of life patient to more appropriate care.
ACO MSSP
-
Risk Scoring and Benchmarking Tools
Dashboards, reporting, and analytics to proactively manage risk scoring, real-time determine benchmark insights to stay top of overall progress to shared savings and improvement opportunities.
-
Quality Improvement
Analytics and dashboards to streamline quality measure reporting and improvement. Driving better decision making and action around quality score improvement across your entire network
-
Leverage Acclivity’s Network of Partners
Use Acclivity’s network of partners (hospice & palliative organizations, doctors, hospitals and other health care service providers) for more streamlined care coordination and transitional care management.
-
Transitional Care Management & Utilization Tools
Transitional Care Management dashboards and workflow to easily uncover and transition patients for a ready for more appropriate care setting (such as a hospice) seamlessly.
Utilization Management Tools
- Gain connections into local HIE sources to know in real-time when a patient is being admitted for an emergency admission, hospital visit, or hospital discharge.
- Notifications are real time, and are sent via email or text message.
- Access predictions of who your potential high utilizers would be for a proactive approach, and which patients are mostly to readmit for a proactive care approach.
Data Aggregation
Data Aggregation For ACOs Explained
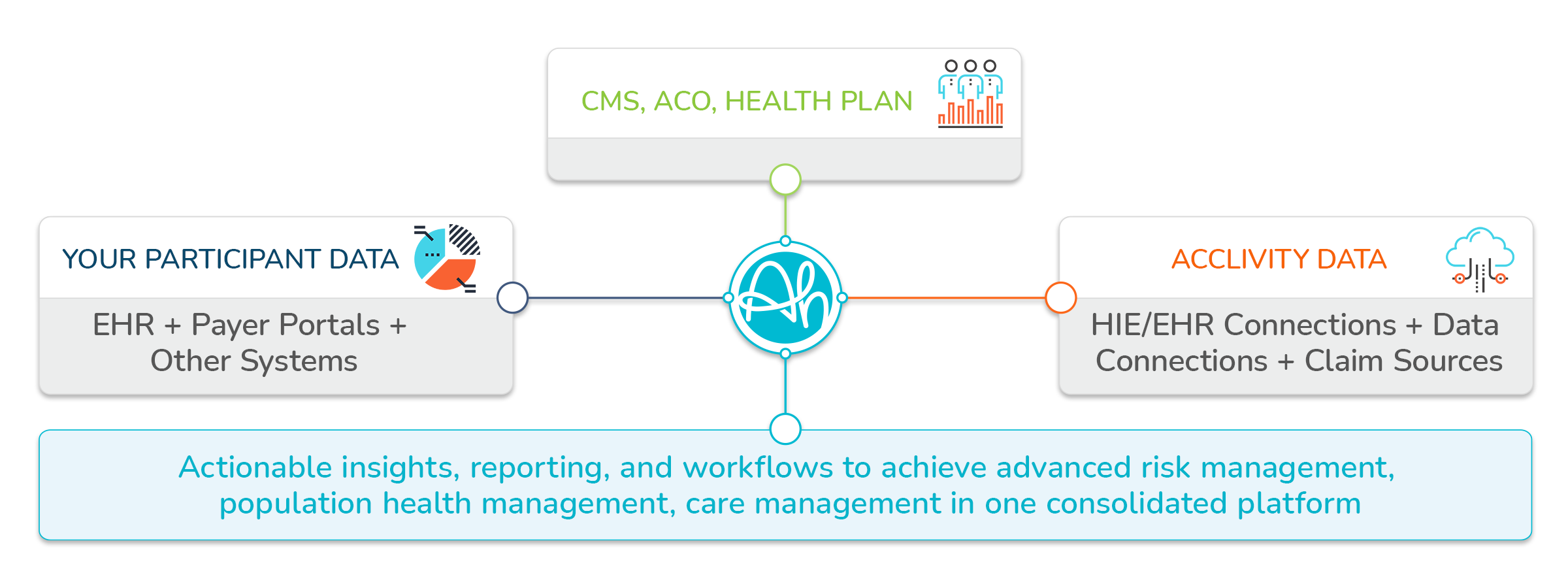
Acclivity combines our data sources with data from your organization and affiliated CMS, ACO, Health Plan, and other key claims sources. This consolidated data enables us to provide you with premier analytics, reporting, and workflows for success within value-based payment models.
Acclivity data sources include:
22 HIE Connections
24 Payer Claim Sources
ACO Data Connections
Post-Acute Data Connections
38 EHR Connections
Your participant data includes:
Medicare Claims
Medicaid Claims
Patient Info
Clinical Data
Financial Data
Provider Data
Labs
Pharmacy
Membership Data
Scheduling Data
The ACO Platform:
Find out more about the 6 ways Acclivity drives value for ACOs MMSP and ACO REACH contracts




