Data Sheet

Value-Based Reporting, Analytics, and Workflow Solutions
Acclivity delivers analytics, administrative reporting, and care management workflows that are crucial for success in risk-based payment models.
-
Value-Based Reporting and Analytics
Success within the alternative payment models start with meaningful reporting and analytics. We provide these in the form of risk management tools, cost analytics, benchmarking, quality measures, social determinants of health insights, utilization metrics, and more.
-
Data Aggregation
We expediently unify all existing data including clinical, social determinants of health, claims, payment, other technologies and more into your EHR. All data is quickly ingested to drive quick action, efficiency, and reduce administrative burden.
-
Patient Flow Management
Turning predictive insights into action. Transitional Care Management & Chronic Care Management workflow to ensure risk is acted upon rather than just uncovered. Plus Annual Wellness Visit insight and workflow to increase patient attribution and daily clinical processes when applicable.
-
Utilization Management and Predictive Tools
- Gain connections into local HIE sources to know in real-time when a patient is being admitted for an emergency admission, hospital visit, or hospital discharge
- Notifications are real time, and are sent via email or text message
- Access predictions of who your potential high utilizers would be for a proactive approach, and which patients are mostly to readmit for a more proactive care approach
-
Clinical Insights and Process Improvement Tool
High-level clinical summary reports and detailed daily patient reports that physicians can access electronically or by print-out before seeing each patient. Key Metrics include Diagnosis, Chronic Conditions, Medications, Total Spend, Pharmacy Spend, SNF use, Social Determinants of Health info, any outside providers or services used, HCC info, Palliative Predictions, Hospitalization history, and so much more.
-
Contract Management Tools & Value-Based Care Experts
Full access to our contract management tools, healthcare economists, actuaries, and value-based care consultants. Plus, access to our full array of post-acute partners to create mutually beneficial transitional care and care coordination arrangements.
Data Aggregation
Data Aggregation for Provider Organizations Explained
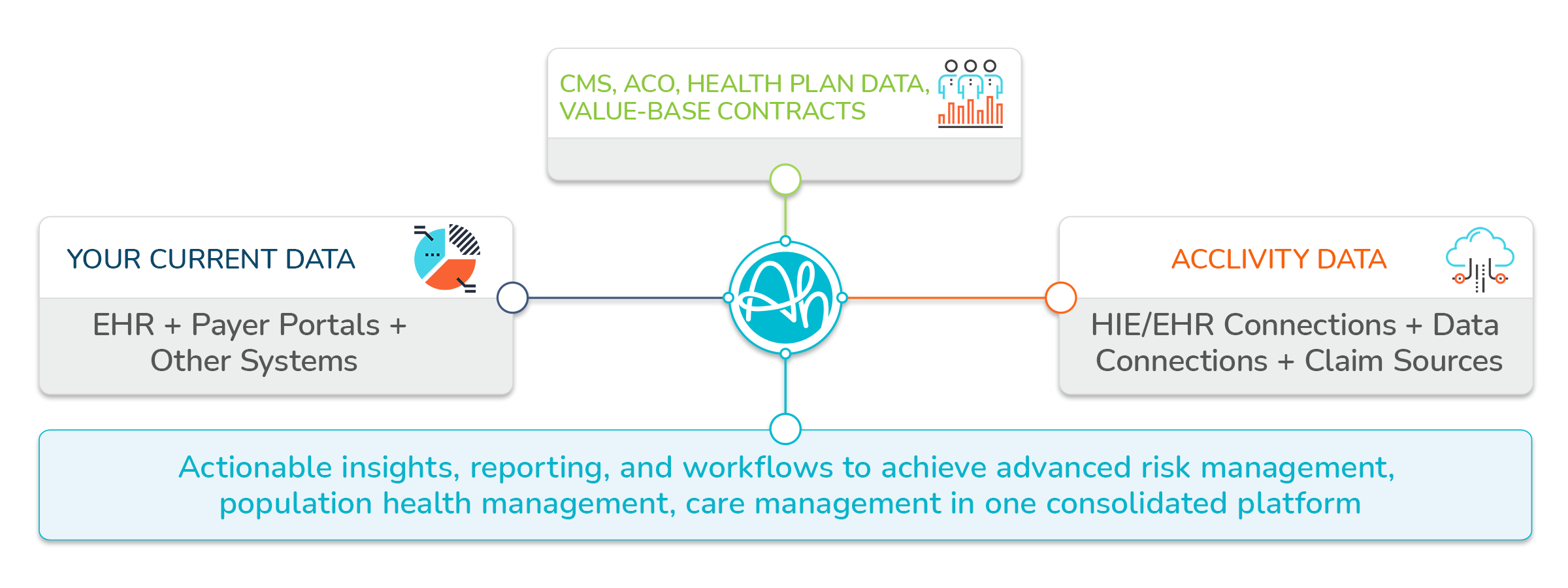
Acclivity combines our data sources with data from your organization and affiliated CMS, ACO, Health Plan, Value-Based Contracts, and other key claims sources. This consolidated data enables us to provide you with premier analytics, reporting, and workflows for success within value-based payment models.
Acclivity data sources include:
22 HIE Connections
24 Payer Claim Sources
ACO Data Connections
Post-Acute Data Connections
38 EHR Connections
Acclivity data sources include:
Medicare Claims
Medicaid Claims
Patient Info
Clinical Data
Financial Data
Provider Data
Labs
Pharmacy
Membership Data
Scheduling Data
The Provider Platform:
Find out more about the 6 ways Acclivity delivers Value-Based Population Health Solutions




